Let Coloradans Decide
Understanding Colorado’s Amendment 79: Protecting Abortion Rights in 2024
Understanding Amendment 79
What would Amendment 79 do?
Passing Amendment 79 would preserve the right to abortion in the Colorado state constitution. This initiative would bar the state or any local government in the state, such as the Pueblo City Council, from blocking the right to an abortion.
Why is this important? I thought Colorado already protected the right to abortion?
Although Colorado passed the Reproductive Health Equity Act in 2022, RHEA enshrines the right to an abortion in state law but not in the state constitution. This means that if a future U.S. president or Congress bans abortion nationwide, Coloradans will lose access to abortion, because federal law overrides state laws.
The Comstock Act and Project 2025
Passing Amendment 79 would enshrine the right to abortion in the Colorado state constitution, safeguarding the reproductive rights of all Coloradans, regardless of what happens if the Comstock Act is implemented or the U.S. Supreme Court issues a ruling regarding fetal personhood. Read more about the Comstock Act and Project 2025.
The Durango Herald editorial board agreed that we need to enshrine the right to abortion in our state constitution, endorsing a YES vote for Amendment 79 in an editorial this September:
“Let’s not let Colorado become one of those uncertain states. It’s best not to involve the government in any questions of reproductive healthcare.
Vote yes on Amendment 79 to affirm Colorado as a state where a woman, along with those closest to her, can make her own decision.”
Stand with someone you love: I support pro-choice federal legislation that ensures abortion access for all.
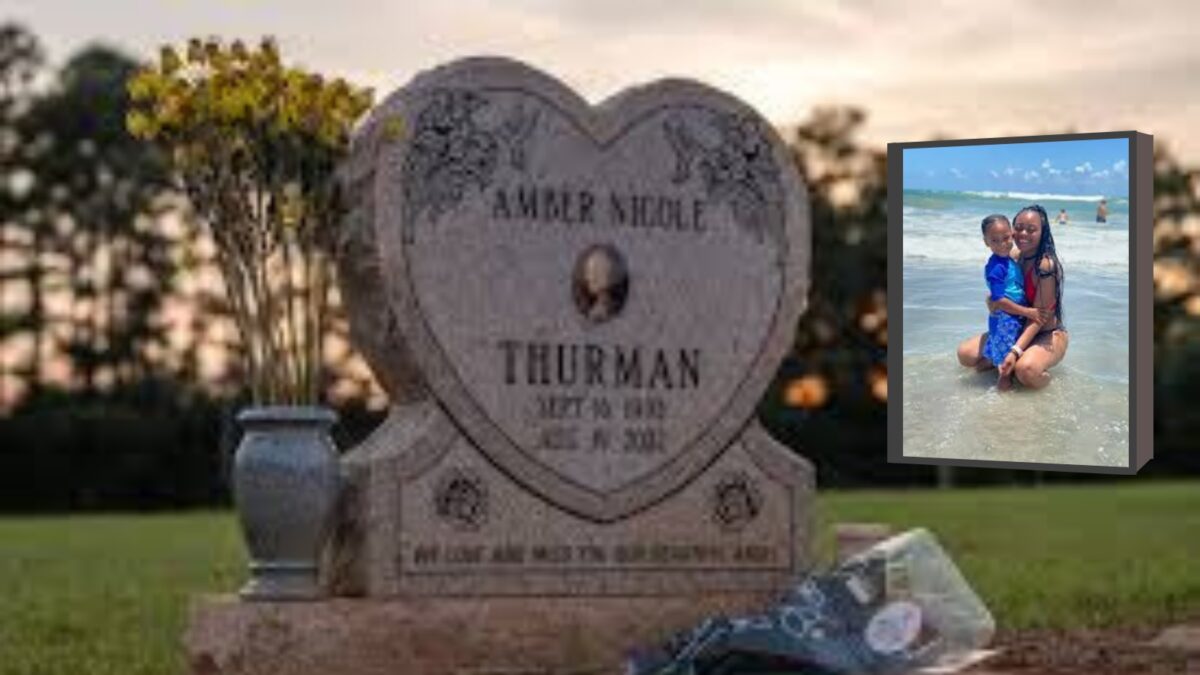
Politicizing Abortion Leads to Tragedies
Recent events in Georgia highlight the devastating effects of restrictive abortion laws. Amber Thurman, a mother and healthcare worker, died after being denied critical care due to Georgia’s abortion ban. The fear of prosecution kept doctors from performing a routine, lifesaving procedure.
There have been multiple documented cases across the U.S. in states like Texas, Idaho, Florida, and Georgia where women were denied emergency abortions, putting their lives at serious risk. One such case involved Anya Cook, a woman in Florida whose water broke at 16 weeks. She was turned away from the hospital, and by the next day, she had lost half the blood in her body. Her husband had to rush her back to the hospital to save her life. Sadly, Anya’s story is not unique–many women across the U.S. who live in states where abortion is heavily restricted or banned have faced similar life-threatening circumstances due to delayed or denied care.
Will Passing Amendment 79 legalize “post-birth abortions?”
Colorado does not allow abortions after birth. The term “abortion” specifically refers to the termination of a pregnancy, which, by definition, applies only before birth. Once a baby is born, any harm to the infant would be governed by laws related to child abuse, neglect, or homicide—not abortion.
What is a “partial-birth abortion,” and will Amendment 79 allow them?
A “partial-birth” abortion is a term made up by the anti-abortion camp to scare people and politicize abortion. There is no such thing as a “partial-birth” abortion. It is not a term recognized by the American Medical Association (AMA) or The American College of Obstetricians and Gynecologists (ACOG).
In fact, in its glossary of medically accurate abortion terminology, ACOG debunks the use of the term “partial-birth abortion:”
“This graphic, inflammatory language is not a medical term and exists to distort the clinical reality. It is vaguely defined in law but is generally interpreted as referring to one method of abortion which occurs later in pregnancy.”
Will this initiative increase “late-term abortions?”
No, “late-term abortion” is not a medically recognized term. This initiative protects the right to abortion in Colorado by enshrining it in the state constitution. This will ensure that doctors can provide necessary care without political interference, including access to care in emergencies to safeguard the patient’s health.
What is a “late-term” abortion?
You may have heard about “late-term,” “partial-birth,” or “post-birth” abortions from politicians, but these are not medically recognized terms.
First and foremost, “post-birth” abortions do not exist. Infanticide–or killing a newborn baby–is illegal in all 50 states and U.S. territories. Many politicians have used this fear-mongering language as a scare tactic to convince voters that doctors are executing babies in maternity wards with parental consent. Don’t be fooled by their extremist talking points.
Although women have abortions for many reasons at different points of pregnancy, there is no such thing as an abortion after birth.
Some women have abortions that are medically necessary, and some have so-called “elective” abortions, another term that is not recognized or backed by science that has been used by politicians interfering in women’s reproductive lives.
Regardless of why you choose to have an abortion, you should be able to get safe and legal medical care without fear of being investigated and accused of a crime.
What do Obstetricians and Perinatologists say about “late-term abortion?”
Katrina Kimport, a professor in the Department of Obstetrics, Gynecology & Reproductive Sciences at the University of California’s ANSIRH program, specializes in researching abortion later in pregnancy, which some politicians and anti-choice extremists like to call “late-term abortion,” which is political, not medical, terminology.
“There’s a heartbreaking number of ways that pregnancy can go wrong,” Kimport has pointed out. There are many situations when a clinical diagnosis of severe fetal anomalies happens at a routine anatomy scan, which is typically scheduled when you’re 20 weeks pregnant.
Dr. Kimport has published several studies about abortions later in pregnancy, or that take place in the third trimester. In one study, 28 women of different races ranging in age from 18 to 46 got abortions at different gestational times between 24 and 35 weeks.
One woman in that study who had already experienced complications with a previous pregnancy was told at 20 weeks that everything was going well. But then at 29 weeks, her healthcare providers detected problems with the fetus’ brain.
Initially, they told her not to worry. But further testing showed parts of her unborn baby’s brain were missing, and perinatologists eventually told her there was no possibility her child would survive. The medical diagnosis was that her fetus was incompatible with life.
According to the Centers for Disease Control (CDC), less than 1% of all abortions in the U.S. happen later in pregnancy at or after 21 weeks of gestation, which is considered the second trimester. The vast majority of abortions–nearly 94%–occur at or before 13 weeks of gestation.
For context, if you are pregnant, your team of healthcare providers will run multiple tests and scans to determine the health and viability of your pregnancy. These tests happen throughout the pregnancy in the first, second, and third trimesters. If medical professionals detect a fetal abnormality, you may decide to have an abortion.
If you get a poor prenatal diagnosis, such as trisomy 18 or trisomy 21 (Down syndrome), or if your healthcare provider determines you have an ectopic pregnancy, you may decide to have an abortion. Some of these fetal abnormalities cannot be detected until the second or even third trimester.
Down syndrome is the most common chromosomal abnormality and is more likely to happen when you are 35 or older. If you live in a state where abortion is illegal, like Florida, Texas, or Alabama, you may not be able to get the care you need.

Kelly Shannon was grieving a pregnancy she decided to terminate because of multiple fetal anomalies, including Down syndrome and a heart defect. She got a call that the second committee of Alabama doctors who reviewed her case refused to approve the abortion, despite the exceptions in the state’s law. That meant she would have to leave Alabama to get an abortion.
According to the CDC, infants with Down syndrome and a heart defect are five times more likely to die in their first year of life than those without, but when facing potential criminal prosecution, the Alabama committee of doctors decided to deny Shannon the care she needed.
Abortion in Colorado
1. What is the current status of abortion in Colorado?
Although the U.S. Supreme Court overturned Roe vs. Wade with the Dobbs decision in 2022, Colorado enacted a statutory protection for abortion as a fundamental right, so abortion continues to be legal across Colorado.
That said, abortion access is not guaranteed by the Colorado state constitution and would be eliminated by a national ban on abortion, which could be implemented by a future presidential administration using the Comstock Act or through a U.S. Supreme Court decision on arguments based on “fetal personhood,” as mapped out in Project 2025. Read more about the Comstock Act and Project 2025.
2. What is Roe vs. Wade?
In 1973, Roe v. Wade made abortion legal in all 50 states. Briefly, Medicaid covered abortions regardless of your age or income. Four years later, Congress passed the Hyde Amendment, which cut abortion coverage out of Medicaid unless the woman’s life was endangered. In 1993, the exception was broadened to pay in cases of rape and incest.
Before the Hyde Amendment, the federal government paid for 1/3 of all abortions; since 1977 it has paid for virtually none.
Now that the U.S. Supreme Court has overturned Roe vs. Wade after more than 50 years as settled law, it has taken away people’s right to control their own reproduction. Anti-choice politicians in Washington, D.C., and across the country have also made clear their plan to pass a federal abortion ban, which would outlaw abortion nationwide. Read more about how anti-choice politicians plan to ban abortion by using the Comstock Act and Project 2025.
3. Will passing Amendment 79 allow minors to get an abortion without parental consent or notification?
This initiative will not change parental involvement laws in the state in any way. According to the Center for Reproductive Rights, Colorado does not require parental consent for minors seeking abortion care; however, the state does require that a parent or legal guardian be notified about their minor child’s care, except in cases where a judge waives the notification requirement.
Keep in mind that most young people facing an unintended pregnancy already turn to a parent or guardian when considering an abortion, and those who don’t will often turn to another trusted adult.
According to a study by Henshaw and Kost, 90% of minors under 15 involved a parent in their decision to have an abortion. Most teens who didn’t talk to a parent turned to another trusted adult.
Let’s be honest, there’s no law that can force families to communicate, nor should lawmakers meddle in how a young woman decides to pursue her reproductive healthcare options.
Additionally, parental involvement laws assume that all young people reside in healthy households with open channels of communication. Not everyone’s home life and family relationships are the same, and this places young people who live in abusive households in dangerous situations.
4. Is abortion taxpayer-funded in Colorado?
No. Passing Amendment 79 is crucial to repeal another constitutional amendment passed by Colorado voters 40 years ago that prohibits taxpayer money, including Medicaid, from being used to pay for abortions. According to The Denver Post, which on October 10 published an editorial endorsing the initiative, passing Amendment 79 “would guarantee all Coloradans have reproductive freedom… (and) provide equitable health care in this state for the thousands of women on Medicaid.”
In its endorsement of Amendment 79, The Denver Post points out:
“The language of Amendment 79 would not prohibit all future regulation of abortion. We know that the most basic constitutional rights can and should have reasonable restrictions placed on them. We have freedom of religion until a cult begins harming people. We have the right to bear arms but not machine guns. We have free speech unless it’s a vicious lie that harms someone’s reputation. Even before five conservative Supreme Court justices stripped pregnant women of their constitutional protections, abortion was heavily regulated across much of the nation at all points of gestation.
If Amendment 79 passes, Coloradans will have the right to have an abortion but lawmakers can ensure those abortions are safe and conducted within the medical best practices recommended by the state’s Board of Health.”
Currently, Colorado bans the use of public funds for abortion, unless it involves a case of rape or incest, or to save the life of the mother. But in many cases, these exceptions simply don’t work.
According to the National Sexual Violence Resource Center, only about 25% of rapes and sexual assaults were reported to police in 2018. Many survivors have expressed that they felt revictimized by police when reporting the assault they experienced, which is why so many women are hesitant to report sexual assaults to the police. Some survivors have even had the tables turned on them by police, becoming the focus of the investigation.
Abortion & Healthcare
1. What is a surgical abortion?
A surgical or procedural abortion is performed in a clinic or hospital by health care providers. If you choose to have a procedural abortion and it has been less than 14 weeks since your last menstruation, your health care provider will perform a vacuum aspiration to end the pregnancy.
Vacuum aspiration is the most common procedural method for abortion early in a pregnancy, and it is extremely safe. According to the University of California’s Advancing New Standards in Reproductive Health (ANSIRH) research program, less than 1% of patients experience a major complication from an abortion.
If you choose to get an abortion and it has been over 14 weeks since your last menstrual cycle, your health care provider will perform a D&E, or dilation and evacuation, which is the most common procedure for abortions at that stage.
2. Are surgical abortions safe for women and girls?
Health experts in Florida, across the country, and worldwide agree that surgical abortions performed by health care providers are safe.
According to ANSIRH, the overall complication rate for abortions is lower than those for having a wisdom tooth removed or having your tonsils removed.
In fact, studies have found that you are 14 times more likely to die from childbirth than from having an abortion.
Similar to a vacuum aspiration, when you have a D&E, the cervix is dilated and the pregnancy is removed through suction.
3. What is a medical abortion?
Also known as a medication abortion, abortion with pills, or plan C, a medical abortion consists of two safe and effective medications that have been FDA-approved for more than two decades.
Although some mistakenly call medication abortions “chemical abortions,” a term that is not recognized by science and has been criticized as fearmongering, the World Health Organization (WHO) has placed these medications on their Essential Medicines List.
4. What is an emergency abortion or a medically necessary abortion?
You could need an emergency abortion at any time during a pregnancy. Health care providers will perform an emergency abortion in different circumstances when abortion is the best way to save your life, health, or fertility in a crisis.
If you have an ectopic pregnancy, go into premature labor before the fetus can survive outside of your body, or health care providers detect that the fetus you are carrying is no longer alive or won’t survive outside your womb, they will most likely have to perform an emergency abortion to stabilize your health and prevent future infertility.
Not surprisingly, nearly 70% of OBGYNs across the country reported that since the U.S. Supreme Court overturned Roe, their ability to manage pregnancy-related emergencies has declined.
A large portion of the OBGYNs surveyed by KFF in June 2023 also believe that the Dobbs decision has worsened pregnancy-related mortality (64%), racial and ethnic inequities in maternal health (70%) and the ability to attract new OBGYNs to the field (55%).
5. What is an ectopic pregnancy?
An ectopic pregnancy occurs when a fertilized egg grows in a location outside of the uterus. This type of pregnancy is nonviable because your body will not support an ectopic pregnancy. If you have an ectopic pregnancy, health care providers will perform an emergency abortion as lifesaving care. According to the American College of Obstetricians and Gynecologists (ACOG):
Almost all ectopic pregnancies—more than 90%—occur outside of the uterine cavity in a fallopian tube, but they can also implant in the abdomen, cervix, ovary, and cesarean scar. An ectopic pregnancy in any location is life threatening. This is because as the pregnancy grows, it can cause the structure where it is implanted to burst, or rupture. A rupture can cause major internal bleeding and is a life-threatening emergency that requires urgent surgery.
6. What is P-PROM?
Premature rupture of membranes (PROM) is when you leak amniotic fluid before labor begins. It’s commonly called your “water breaking.” If it happens after 37 weeks of pregnancy, your health care provider can deliver your baby.
If it happens earlier, it is commonly called preterm premature rupture of membranes or P-PROM. If your water breaks before 37 weeks of the pregnancy, your health care provider must weigh the risk of premature birth against the risks of complications and risks to your health and future fertility, such as an infection.
When your water breaks very early in the pregnancy, like in the case of Anya Cook in Florida, health care providers must be able to perform an emergency abortion to prevent sepsis and other complications that could cost you your life, health, or future fertility.
But Cook, who went to a local hospital after her water broke in her second trimester at 16 weeks, was discharged from the emergency room because she was not sick enough to qualify for the emergency medical exception in Florida’s abortion law, despite her risk for infection and hemorrhage.
Shanae Smith-Cunningham, who also lives in South Florida, had a similar experience. Smith-Cunningham was turned away from a local emergency room when her water broke at 19 weeks.
Both Cook and Smith-Cunningham had planned, wanted pregnancies and had experienced prior miscarriages. Both almost died from complications after being denied emergency abortions.
7. What is trisomy 18?
Trisomy 18, also known as Edwards Syndrome, is a genetic disorder in which a fetus has an extra copy of chromosome 18. The causes for trisomy 18 are unknown, but specialists do know that it occurs at the time of conception.
According to Cleveland Clinic, trisomy 18 occurs in one in 5,000 to 6,000 live births, but this genetic disorder is much more common in pregnancy, occurring in one in approximately 2,500 pregnancies.
That’s because at least 95% of fetuses diagnosed with trisomy 18 don’t survive to full term, as these pregnancies end in miscarriage or babies that are stillborn.
There is no cure for trisomy 18. Almost all pregnancies with this diagnosis end in a miscarriage or stillbirth. Of those pregnancies surviving into the third trimester, nearly 40% of babies diagnosed with trisomy 18 don’t survive labor.
The survival rate varies for babies born with trisomy 18:
-Between 60% and 75% survive to their first week.
-Between 20% and 40% survive to their first month.
-Less than 10% survive past their first year.
If you have a child born with trisomy 18, he or she will need specialized care immediately after they are born, and for the rest of their short lives.
8. How much does an abortion cost?
An abortion can cost anywhere between hundreds of dollars ($600+) to thousands of dollars, depending on the type of abortion–procedural or medication–and where you are getting care.
This represents the cost of the abortion itself, but you need to also consider other expenses, such as time off work to have the procedure; childcare, if you are already a parent; travel and lodging costs, if you need to travel outside of your area to find a clinic.
9. Can I get an abortion via telehealth in Colorado?
Yes. You can get a prescription for abortion medication via telehealth from physicians, nurse practitioners, and physician assistants in the first 10 weeks of a pregnancy. Typically, telehealth providers will require that you be physically present in Colorado during the telehealth consultation and that you provide a Colorado mailing address for delivery of the abortion medication. You can read more information about your reproductive rights in Colorado from the state attorney general’s office.
10. What is a self-managed abortion (SMA)?
A self-managed abortion is a medication abortion with mifepristone and misoprostol or with misoprostol alone that you take at home or in a place of your own choosing.
According to the World Health Organization (WHO):
In the first 12 weeks of pregnancy, a medical abortion can also be safely self-managed by the pregnant person outside of a health care facility (e.g. at home), in whole or in part. This requires that the woman has access to accurate information, quality medicines and support from a trained health worker (if she needs or wants it during the process).
The WHO explains that “With appropriate support, women can self-manage some or all stages of a medical abortion in the comfort of their own home.”
Based on the WHO’s guidance, you can safely manage a medication abortion at home with mifepristone and misoprostol or with misoprostol alone up to about 12 weeks into a pregnancy.
The Abortion Pill
1. What is the abortion pill?
Abortion pills, or medication abortion, are a safe and effective way to end a pregnancy up to 11 weeks gestation, and they’ve been approved by the FDA for over two decades. They are a combination of two medications that help end the pregnancy. If you terminate a pregnancy using medication abortion, you are likely to experience cramping and bleeding in the days following the abortion with pills.
2. How does the abortion pill work?
The first medicine, mife, which is usually taken in one dose of 200 milligrams, blocks a hormone called progesterone that is needed for the pregnancy to continue. You then take the second medication, miso, within 24 to 48 hours. The miso expels the fetal tissue from your uterus. You can also take a different dose of miso alone to end a pregnancy.
You can follow up with a healthcare provider one to two weeks after taking the first dose, or earlier, if you are experiencing unusual symptoms like excessive bleeding or hemorrhaging.
3. Is the abortion pill safe?
Mife and miso are very safe. The FDA first approved the generic version 25 years ago, and this medication has an extensive record of safety and effectiveness without major complications.
About 6 million women have taken mife since it was first approved by the FDA. There have been only 32 deaths reported to the FDA of women who used the drug to terminate a pregnancy through 2022; however, that figure includes all deaths, not just those in which the medication played a role.
Recent reports from ProPublica found that only 11 of those deaths were linked to mife. The majority of those deaths were due to overdoses, suicide, homicide, or ruptured ectopic pregnancies, not the abortion pill.
Additionally, the World Health Organization (WHO) includes both mife and miso in their Essential Medicines List.
According to Dr. Bela Ganatra, head of the Comprehensive Abortion Care Unit at the WHO:
“Medical abortion has played a seminal role in expanding access to safe abortion globally, especially for women and girls in the most vulnerable situations who may lack access to health facilities or need to keep their abortion private by avoiding hospital stays, so it’s important that healthcare practitioners can facilitate it as an option for abortion care.”
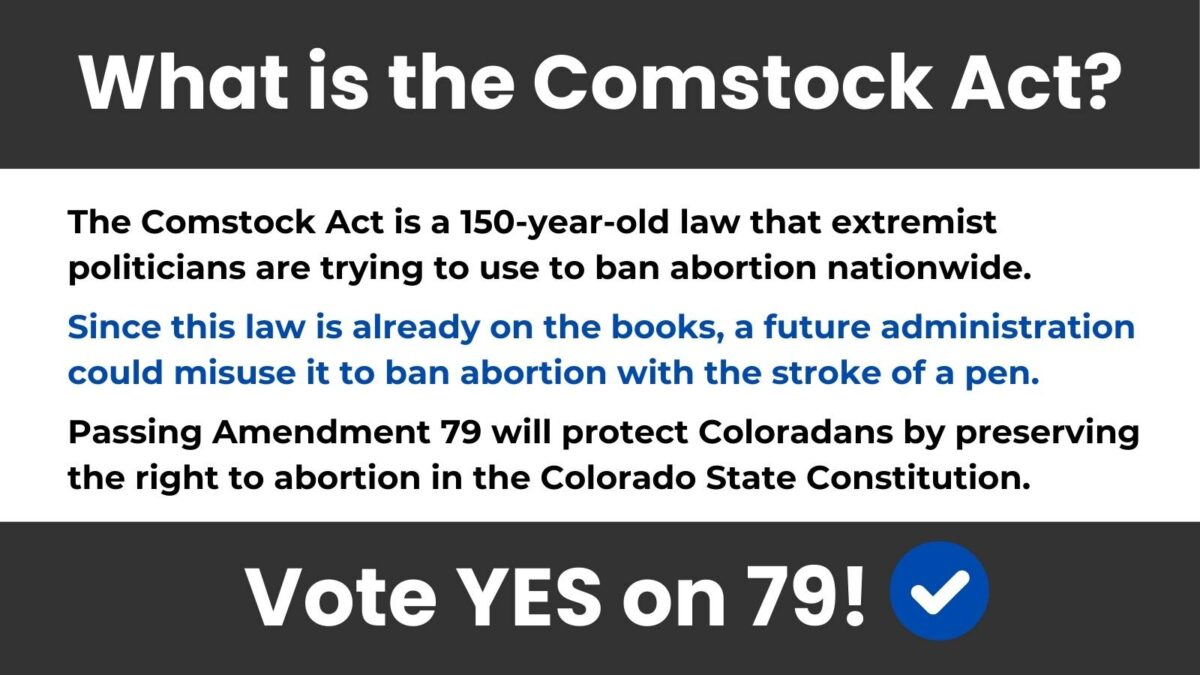
The Comstock Act
1. I thought abortion access was safe in Colorado? Why do we need Amendment 79?
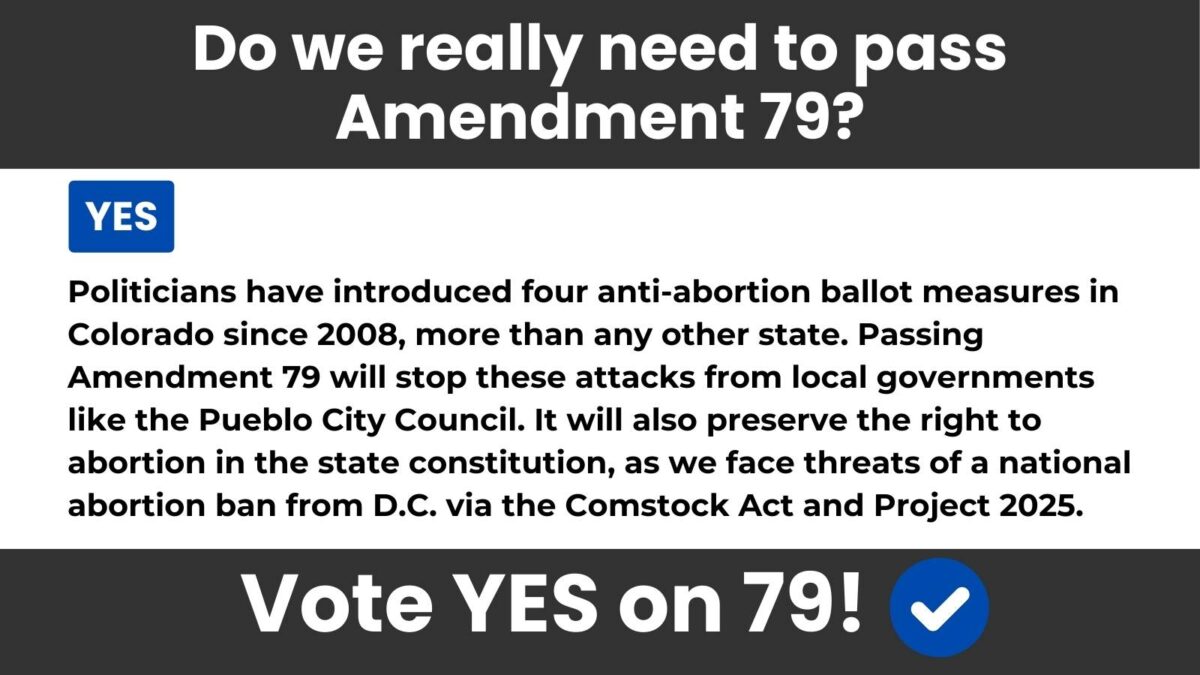
Coloradans need Amendment 79 for two reasons: to stop Colorado politicians from attacking abortion rights and to form a line of defense against the Comstock Act and Project 2025.
Colorado politicians try to ban abortion in Colorado every election.
There have been four anti-abortion ballot measures introduced in the state since 2008, eight total since 1984, more than any other state.
Following the Dobbs decision that overturned Roe v. Wade, the architects of Texas’ SB8, the abortion ban that put a bounty on abortion providers, attempted to pass a municipal abortion ban in Pueblo, CO, by invoking the Comstock Act. Although they failed, these attacks will continue without a state constitutional amendment.
Voting Yes on Amendment 79 will put an end to politicians’ constant attempts to make abortion illegal in Colorado.
2. What is the The Comstock Act?
The Comstock Act is a 150-year-old law that prohibits “explicit” materials from being mailed. However, the definition of “explicit” in the law is so broad that MAGA Republicans are trying to use Comstock to ban abortion pills from being sent in the mail and justify municipal abortion bans like the one they tried to pass in Pueblo, CO. Their plan to use Comstock to make abortion illegal is all there, written in black in white, in Project 2025. But there’s more.
Under Comstock, politicians, no matter their party, can use this outdated law to ban anything they deem explicit or offensive from being sent through the mail. That could include HIV medication, LGBTQ+ history books, women’s history books, and so much more.
Until the Comstock Act is fully repealed, states like Colorado will need to form a firm line of defense against it to keep abortion legal and accessible.
Voting Yes on Amendment 79 will protect Coloradans’ right to abortion while the Comstock Act is still on the books.
Pueblo City Council
Time after time, Coloradans have voted for personal choice over government interference when it comes to our important healthcare decisions, like abortion.
In 2022, after the U.S. Supreme Court overturned Roe vs. Wade, eliminating all federal protections for the right to abortion, Coloradans passed the Reproductive Health Equity Act (RHEA), which guarantees the right to abortion in state law.
But federal law overrides state law, which is why we need to enshrine the right to abortion in the Colorado State Constitution. Abortion is not protected in the Colorado Constitution and remains vulnerable to extremists. Anti-choice politicians in Washington, D.C., and even in our own state, continue to wage relentless attacks against our bodily autonomy.

Extremist politicians on the Pueblo City Council continue to attack abortion access with ordinances meant to silence reproductive health advocates and punish women who seek abortions, doctors who provide healthcare, and anyone who helps a friend, neighbor, or loved one get an abortion.
In fact, a Pueblo City Councilor threatened to introduce another anti-abortion ordinance in September 2024, after trying to make Pueblo a “sanctuary for the unborn” with an ordinance that invoked the Comstock Act in an effort to stop the CARE clinic from opening in Pueblo.
Politicians try to ban abortion in Colorado every election. There have been four anti-abortion ballot measures introduced in the state since 2008, eight total since 1984, more than any other state.
After Roe v. Wade was overturned, the architects of Texas’ SB8 abortion ban, which encourages Texans to sue abortion providers and anyone who helps someone access abortion for up to $10,000 each, attempted to pass a municipal abortion ban in Pueblo by invoking the Comstock Act. They failed, but these attacks will continue without a constitutional amendment.
These extremists have even gone so far as to bus in dozens of anti-abortion radicals from Texas to make it seem as though these attacks have support from a large segment of Coloradans. They don’t.
Now, just weeks before the election, The Pueblo Chieftain published excerpts from an email sent by a statewide anti-abortion group calling on two new members of the Pueblo City Council to reintroduce this ordinance, which has already failed twice, seeking to abolish abortion in Pueblo and make it a “Sanctuary City for the Unborn.”
In the email, the group writes “Fast forward two years, and there are new city council members who were elected because of their pro-life beliefs. With a majority on the council, the ordinance was reintroduced this week but FAILED because two of the new council members voted against it, even though they were voted into office specifically to move this forward.”

According to the local publication, which has access to the communications, the email urges individuals throughout Colorado to “flood” the email inboxes of the two council members and demand that they “stand by their pro-life values to reintroduce and pass this ordinance.”
Passing Amendment 79 will effectively block these relentless attacks and preserve the right to abortion in the Colorado State Constitution. It will protect abortion access, not just from federal threats like a national ban brought about at the stroke of a pen by a future president using the Comstock Act, but from radicals in the state who see Texas as a model for eliminating all abortion access in Colorado.
“Pregnancy Resource Centers”
1. What is a “Pregnancy Resource Center” or “Crisis Pregnancy Center (CPC)”?
With more than 50 fake pregnancy resource centers in Colorado, anti-abortion extremists have a hold on every community. Even though they are sometimes called “Crisis Pregnancy Centers” or CPCs, you cannot get comprehensive pregnancy care at these fake clinics–or much of any health care at all!
They also like to call themselves “Pregnancy Help Clinics” or even “Pregnancy Medical Clinics,” but they’re not medical clinics at all, and they don’t help women. They use shady tactics to dissuade you from using contraceptives and seeking abortion.
It is important to be aware of these so-called “Pregnancy Resource Centers” that present themselves as resources for women and girls facing unplanned pregnancies. These centers will not provide or refer you to get an abortion.
These fake clinics are often deliberately located near actual reproductive health clinics. They create websites that appear in online searches for legitimate abortion clinics and advertise online and in print media in ways that might appeal to those who are considering abortion.
These anti-choice centers also may delay scheduling appointments, thereby preventing you from getting an abortion earlier in pregnancy, sometimes delaying for so long that getting an abortion becomes more difficult, expensive, and in some cases, impossible.
So-called “Pregnancy Help Centers” are typically managed and funded by organizations that oppose abortion in any and all circumstances. As a result, if you have an unintended pregnancy and are seeking full options for counseling or abortion referrals, they will not help you.
2. How can you tell if a clinic actually provides abortions?
Check the clinic’s website for statements about whether or not it provides abortions. Often, disclosure that the so-called “Pregnancy Resource Center” does not provide abortions or referrals is hidden in small print on its website.
You can call the clinic and ask them directly if they offer abortions and what type of abortions they offer (medical with pills or procedural), and see if the clinic seems to hesitate or avoid answering your direct questions.
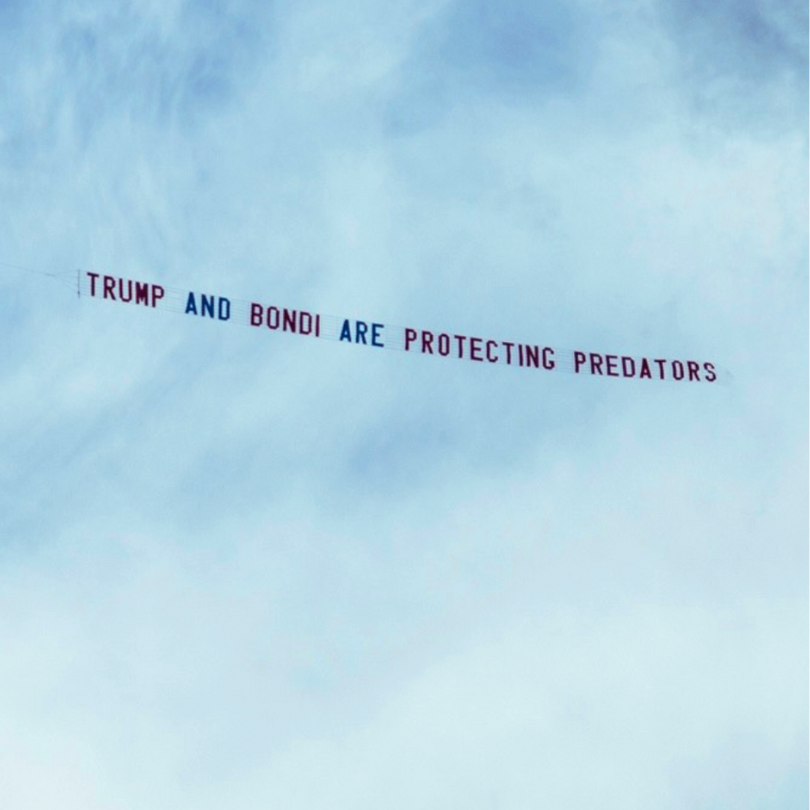
Give for survivor justice taking flight!
While Donald Trump and Pam Bondi want to change the subject, we refuse to let them off the hook for protecting predators. That’s why we're flying airplane banners to keep Trump’s ties to child sex abuser and trafficker Jeffrey Epstein in the news. Epstein’s more than 1,000 survivors deserve transparency and justice. Your gift today will keep the spotlight on Trump’s and Bondi’s deflections and center survivors in the public narrative!